The Most Abundant Cation In Extracellular Fluid Is
Kalali
Mar 10, 2025 · 6 min read
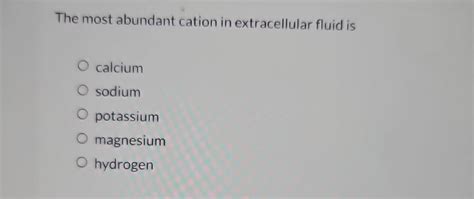
Table of Contents
The Most Abundant Cation in Extracellular Fluid Is: Sodium (Na+) – A Deep Dive into its Role and Significance
The human body is a complex symphony of interconnected systems, each dependent on a precise balance of various components. One crucial aspect of this intricate balance is the electrolyte composition of bodily fluids. Understanding the precise roles of these electrolytes is fundamental to comprehending overall health and disease. This article delves deep into the most abundant cation in extracellular fluid: sodium (Na+), exploring its crucial functions, regulatory mechanisms, and the implications of imbalances.
Sodium's Predominance in Extracellular Fluid
Extracellular fluid (ECF) encompasses the fluid surrounding cells, including interstitial fluid (between cells) and plasma (liquid component of blood). Maintaining the correct balance of electrolytes within this fluid is paramount for numerous physiological processes. While several cations (positively charged ions) are present in ECF, sodium ions (Na+) reign supreme, significantly outnumbering other cations like potassium, calcium, and magnesium. This dominance dictates several key physiological roles.
Why is Sodium so Abundant?
The high concentration of sodium in ECF is not accidental; it's a result of active and finely tuned regulatory mechanisms. The body actively maintains this concentration through:
-
Sodium-Potassium Pump (Na+/K+ ATPase): This vital enzyme, located in cell membranes, actively transports sodium out of cells and potassium into cells. This constant pumping contributes significantly to the higher sodium concentration outside cells.
-
Renal Regulation: The kidneys play a crucial role in maintaining sodium balance by adjusting the amount of sodium excreted in urine. This regulation is influenced by hormones like aldosterone, which promotes sodium reabsorption in the kidneys.
-
Dietary Intake: Our sodium intake significantly impacts ECF sodium levels. A diet high in sodium leads to increased ECF sodium, while a low-sodium diet results in lower levels.
Crucial Roles of Sodium in the Body
The high concentration of sodium in ECF isn't merely a coincidental occurrence; it underpins several essential physiological processes:
1. Maintaining Fluid Balance (Osmosis):
Sodium plays a pivotal role in regulating fluid balance through osmosis. Sodium's concentration gradient across cell membranes influences water movement. Water tends to move from areas of low solute concentration (high water concentration) to areas of high solute concentration (low water concentration). Because sodium is the most abundant cation in ECF, it significantly influences the osmotic pressure, dictating the distribution of water between the intracellular and extracellular compartments. This is vital for maintaining cell volume and preventing cell swelling or shrinkage.
2. Nerve Impulse Transmission:
Sodium is crucial for the propagation of nerve impulses. The rapid influx of sodium ions into nerve cells triggers depolarization, initiating the action potential that transmits signals along nerve fibers. This process underpins all neural activity, from simple reflexes to complex cognitive functions. Disruptions in sodium balance can significantly impair nerve conduction, leading to neurological symptoms.
3. Muscle Contraction:
Similar to nerve impulse transmission, sodium ions play a vital role in muscle contraction. The influx of sodium into muscle cells contributes to the depolarization of muscle cell membranes, initiating the events leading to muscle fiber contraction. This is essential for movement, respiration, and other bodily functions.
4. Nutrient Absorption:
Sodium is involved in the absorption of certain nutrients, such as glucose and amino acids, from the digestive tract. The co-transport of these nutrients with sodium across the intestinal epithelial cells facilitates efficient nutrient uptake.
5. Blood Pressure Regulation:
Sodium plays a crucial role in blood pressure regulation. Elevated sodium levels increase the volume of extracellular fluid, which in turn increases blood volume. This increased blood volume can lead to elevated blood pressure. Conversely, low sodium levels can result in decreased blood volume and potentially low blood pressure. This close relationship highlights the importance of maintaining appropriate sodium levels for cardiovascular health.
Consequences of Sodium Imbalance
Maintaining a precise balance of sodium in ECF is crucial. Deviations from this balance, whether hyponatremia (low sodium) or hypernatremia (high sodium), can lead to serious health consequences.
Hyponatremia (Low Sodium):
Hyponatremia, characterized by abnormally low sodium levels in the blood, can result from various causes, including excessive sweating, diarrhea, vomiting, kidney disorders, and certain medications. Symptoms can range from mild (headache, nausea) to severe (seizures, coma). The severity of symptoms depends on the rate and extent of sodium depletion. Treatment focuses on correcting the underlying cause and gradually restoring sodium levels to normal.
Hypernatremia (High Sodium):
Hypernatremia, conversely, signifies abnormally high sodium levels in the blood. It commonly stems from dehydration (inadequate fluid intake), excessive sodium intake, or impaired kidney function. Symptoms include thirst, confusion, seizures, and coma. Treatment involves careful rehydration and correcting the underlying cause. Rapid correction of hypernatremia can be dangerous, necessitating slow and controlled rehydration.
Sodium Intake and Dietary Recommendations
Dietary sodium intake significantly influences ECF sodium levels. Excessive sodium intake, often associated with processed foods, fast food, and salty snacks, contributes to hypertension (high blood pressure) and increases the risk of cardiovascular diseases, stroke, and kidney disease. Therefore, maintaining a balanced sodium intake is crucial for overall health.
Dietary guidelines generally recommend limiting daily sodium intake to less than 2,300 milligrams (mg) per day, with even lower intakes (less than 1,500 mg per day) recommended for certain individuals, such as those with hypertension or kidney disease. Reading food labels, choosing low-sodium options, and preparing meals at home are effective strategies for reducing sodium intake.
Advanced Considerations: Hormonal Regulation and Renal Mechanisms
The precise control of ECF sodium involves intricate hormonal and renal mechanisms working in concert.
-
Renin-Angiotensin-Aldosterone System (RAAS): This hormonal system plays a vital role in regulating sodium balance. When blood volume or blood pressure decreases, the kidneys release renin, which triggers a cascade of events leading to the production of aldosterone. Aldosterone promotes sodium reabsorption in the kidneys, increasing blood volume and blood pressure.
-
Atrial Natriuretic Peptide (ANP): In contrast to the RAAS, ANP is released from the heart in response to increased blood volume and stretches the atria. ANP promotes sodium excretion, lowering blood volume and blood pressure.
-
Renal Sodium Handling: The kidneys are the primary regulators of sodium excretion. They adjust sodium reabsorption and excretion based on various factors, including blood volume, blood pressure, and hormonal signals. The nephrons, the functional units of the kidneys, play a critical role in this process.
Conclusion: The Significance of Sodium Balance
Sodium, the most abundant cation in extracellular fluid, is an essential electrolyte with far-reaching physiological implications. Its role in maintaining fluid balance, nerve impulse transmission, muscle contraction, nutrient absorption, and blood pressure regulation highlights its vital importance. Maintaining appropriate sodium levels through a balanced diet and addressing underlying medical conditions is critical for preserving overall health and preventing serious complications. The intricacies of sodium regulation, involving the interplay of various hormonal and renal mechanisms, underscore the remarkable sophistication of the human body's homeostatic control. A deeper understanding of these mechanisms provides valuable insights into the maintenance of overall health and treatment of imbalances. Understanding the role of sodium is fundamental to both preventative healthcare and effective treatment of related pathologies.
Latest Posts
Latest Posts
-
What Is The Hottest Color Star
Mar 10, 2025
-
One Eighth Of An Ounce Is How Many Grams
Mar 10, 2025
-
How Many Ml Is 10 5 Oz
Mar 10, 2025
-
Antiderivative Of Square Root Of X
Mar 10, 2025
-
180 Kilometers To Miles Per Hour
Mar 10, 2025
Related Post
Thank you for visiting our website which covers about The Most Abundant Cation In Extracellular Fluid Is . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
