Where Is The Sugar Removed From The Blood
Kalali
Mar 11, 2025 · 5 min read
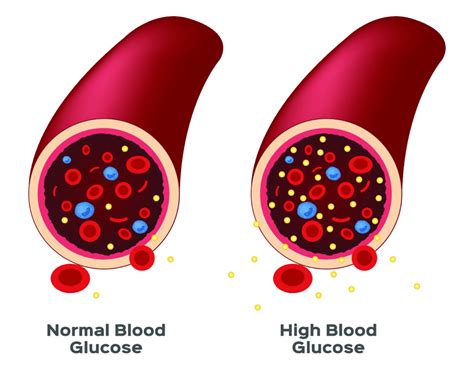
Table of Contents
Where is Sugar Removed from the Blood? The Intricate Process of Glucose Regulation
Maintaining stable blood sugar levels is crucial for our overall health and well-being. Hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar) can both lead to serious health complications. Understanding how our bodies regulate blood glucose, and specifically, where the sugar is removed, is key to appreciating this complex process. This article delves into the intricate mechanisms involved, focusing on the role of the pancreas, liver, and muscles in regulating blood glucose levels.
The Pancreas: The Maestro of Blood Sugar Regulation
The pancreas, a small organ nestled behind the stomach, plays a central role in blood sugar control. It houses two crucial cell types within the islets of Langerhans: alpha cells and beta cells. These cells produce hormones that have opposing effects on blood glucose:
Beta Cells and Insulin: The Blood Sugar Lowerers
When blood glucose levels rise after a meal, beta cells in the pancreas release insulin. Insulin acts like a key, unlocking the doors of cells throughout the body, allowing glucose to enter. This process is crucial because glucose is the primary fuel source for our cells. Without insulin, glucose cannot enter the cells, leading to a buildup of glucose in the bloodstream – hyperglycemia.
Where does insulin work its magic? Insulin's effects are widespread:
- Muscle cells: Muscles are significant glucose consumers, particularly during exercise. Insulin stimulates glucose uptake by muscle cells, helping to lower blood sugar levels. This is a major site of glucose removal from the blood.
- Liver cells (hepatocytes): The liver plays a dual role in glucose metabolism. Insulin signals the liver to take up glucose from the blood and store it as glycogen, a form of stored glucose. This process is called glycogenesis.
- Fat cells (adipocytes): Insulin promotes glucose uptake by fat cells and its conversion into triglycerides, a form of energy storage. This helps to prevent excess glucose from circulating in the blood.
Alpha Cells and Glucagon: The Blood Sugar Raisers
When blood glucose levels drop too low (hypoglycemia), alpha cells in the pancreas release glucagon. Glucagon has the opposite effect of insulin; it signals the liver to break down glycogen stores and release glucose back into the bloodstream, raising blood sugar levels. This process is called glycogenolysis.
The Liver: The Blood Sugar Buffer
The liver isn't just a passive recipient of insulin and glucagon signals. It acts as a crucial buffer, regulating blood glucose levels by performing several key functions:
Glycogenesis: Storing Glucose for Later
As mentioned above, the liver stores excess glucose as glycogen. This stored glycogen acts as a reservoir, providing glucose when blood sugar levels drop. This process is primarily driven by insulin.
Glycogenolysis: Releasing Glucose When Needed
When blood glucose levels are low, glucagon signals the liver to break down glycogen into glucose and release it into the bloodstream. This process is vital for maintaining blood sugar levels during periods of fasting or exercise.
Gluconeogenesis: Creating Glucose from Scratch
In prolonged fasting or starvation, the liver can even create glucose from non-carbohydrate sources, such as amino acids (from proteins) and glycerol (from fats). This process, called gluconeogenesis, is crucial for preventing dangerously low blood sugar levels.
Muscles: Glucose Consumers and Energy Stores
Skeletal muscles are significant consumers of glucose, particularly during exercise. Insulin facilitates glucose uptake into muscle cells, where it's used to generate energy (ATP) through cellular respiration. This process is a major mechanism for removing glucose from the bloodstream.
Muscles also store a small amount of glycogen, which can be used as an immediate energy source during exercise. However, unlike the liver, muscle glycogen is primarily used locally and doesn't contribute significantly to overall blood glucose regulation.
Kidneys: The Last Resort for Glucose Removal
Under normal conditions, the kidneys don't play a major role in glucose regulation. The kidneys efficiently reabsorb glucose from the filtrate produced during urine formation. However, when blood glucose levels are extremely high (as in uncontrolled diabetes), the kidneys' reabsorption capacity is exceeded. Excess glucose spills over into the urine (glycosuria), leading to significant glucose loss. This is a sign of poorly controlled diabetes and can lead to dehydration and other complications.
Hormonal Influences Beyond Insulin and Glucagon
Several other hormones influence blood glucose levels:
- Cortisol: A stress hormone that increases blood glucose levels by stimulating gluconeogenesis in the liver.
- Epinephrine (Adrenaline): A hormone released during stress or exercise that increases blood glucose levels by promoting glycogenolysis in the liver and muscles.
- Growth Hormone: A hormone that promotes growth and has both glucose-raising and glucose-lowering effects depending on the context.
The Role of Diet and Exercise
Our diet and exercise habits significantly impact blood glucose regulation. A diet high in refined carbohydrates and sugars can lead to rapid spikes in blood glucose, placing a greater burden on the pancreas and other regulatory systems. Regular exercise improves insulin sensitivity, making cells more responsive to insulin and improving glucose uptake.
Blood Sugar Monitoring and Management
Regular blood sugar monitoring is essential for individuals with diabetes or those at risk of developing diabetes. This helps in managing blood sugar levels effectively, preventing complications, and improving overall health.
Understanding the Complexities: Diabetes and Blood Sugar Dysregulation
Diabetes is a group of metabolic disorders characterized by hyperglycemia. Type 1 diabetes is an autoimmune disease where the body's immune system destroys the beta cells in the pancreas, leading to insulin deficiency. Type 2 diabetes is characterized by insulin resistance, where cells become less responsive to insulin's effects. In both types, glucose cannot enter the cells effectively, resulting in high blood glucose levels.
Conclusion: A Delicate Balance
The removal of sugar from the blood is a finely tuned process involving multiple organs, hormones, and metabolic pathways. The pancreas, liver, muscles, and kidneys all play crucial roles in maintaining blood glucose homeostasis. Understanding this complex interplay is essential for preventing and managing conditions like diabetes and ensuring overall health. A balanced diet, regular exercise, and appropriate medical intervention (if needed) are vital for maintaining healthy blood sugar levels. This intricate system, when functioning optimally, ensures that our bodies have the energy they need to thrive. Dysfunction in any part of this system can lead to serious health consequences, highlighting the importance of maintaining a healthy lifestyle and seeking medical attention when necessary.
Latest Posts
Latest Posts
-
How Many 12 Oz Cups In A Gallon
Jul 12, 2025
-
How Much Older Is John The Baptist Than Jesus
Jul 12, 2025
-
How Many Teaspoons In A Pound Of Sugar
Jul 12, 2025
-
How Do You Pass Level 12 On Bloxorz
Jul 12, 2025
-
How Far Is 0 4 Miles To Walk
Jul 12, 2025
Related Post
Thank you for visiting our website which covers about Where Is The Sugar Removed From The Blood . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.