Why Is The Action Of Phagocytes Considered A Nonspecific Response
Kalali
Mar 17, 2025 · 6 min read
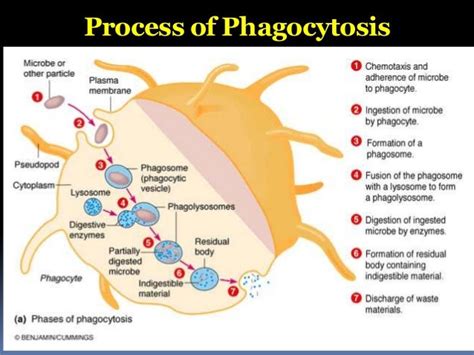
Table of Contents
Why is the Action of Phagocytes Considered a Nonspecific Response?
The human body is a remarkable fortress, constantly battling an unseen war against a vast army of pathogens. Our immune system, a complex network of cells and processes, is our primary defense. Within this system, phagocytes stand as the frontline soldiers, engulfing and destroying invaders. However, a key characteristic of phagocytic action is its nonspecificity. This means phagocytes don't target specific pathogens; instead, they respond to a broad range of threats. This article delves deep into the reasons why the action of phagocytes is considered a nonspecific response, exploring the mechanisms involved and contrasting it with the specific immune response.
Understanding Phagocytosis: The Cellular Pac-Man
Phagocytosis, the process by which phagocytes engulf and digest foreign particles, is a fundamental aspect of innate immunity. Phagocytes, including macrophages, neutrophils, and dendritic cells, are equipped with specialized receptors on their cell surfaces that recognize patterns associated with pathogens, but not the pathogens themselves. This recognition is crucial, yet nonspecific, enabling a rapid and widespread response to infection. Think of it like a security guard who isn't trained to identify specific criminals but can recognize suspicious behavior – a threat, regardless of the specifics.
The Key Players: Types of Phagocytes
-
Macrophages: These are large, long-lived phagocytes residing in tissues throughout the body. They act as sentinels, constantly surveying their environment for pathogens and cellular debris. Their role extends beyond phagocytosis; they also present antigens to initiate the adaptive immune response, bridging the gap between innate and acquired immunity.
-
Neutrophils: These are the most abundant type of white blood cell and the first responders to infection. They are highly mobile and quickly migrate to sites of inflammation, where they engulf and destroy bacteria and other pathogens. Their lifespan is shorter than macrophages, often undergoing apoptosis (programmed cell death) after phagocytosis.
-
Dendritic cells: Located primarily in tissues exposed to the environment (like the skin and mucous membranes), these phagocytes act as a critical link between the innate and adaptive immune systems. They capture antigens from pathogens and migrate to lymph nodes, presenting them to T cells, initiating the specific immune response.
The Mechanism of Nonspecific Phagocytosis: Recognizing Danger Signals
Phagocytes don't possess the sophisticated recognition mechanisms of the adaptive immune system, which targets specific antigens. Instead, they rely on the recognition of pathogen-associated molecular patterns (PAMPs). PAMPs are conserved molecular structures found on a wide variety of pathogens, but not on host cells. These include:
- Lipopolysaccharide (LPS): A major component of the outer membrane of Gram-negative bacteria.
- Peptidoglycan: A key component of bacterial cell walls.
- Flagellin: A protein found in bacterial flagella.
- Lipoteichoic acid: Found in the cell walls of Gram-positive bacteria.
- Double-stranded RNA (dsRNA): A characteristic of many viruses.
Phagocytes possess pattern recognition receptors (PRRs), such as Toll-like receptors (TLRs), that bind to these PAMPs. This binding triggers a signaling cascade that leads to:
- Chemotaxis: Phagocytes are attracted to the site of infection by chemotactic signals, such as chemokines and complement proteins.
- Adherence: The phagocyte adheres to the pathogen via its receptors. Opsonins, such as antibodies and complement proteins, can enhance adherence. This process is called opsonization.
- Ingestion: The phagocyte extends pseudopods (cytoplasmic projections) that engulf the pathogen, forming a phagosome (a membrane-bound vesicle).
- Digestion: The phagosome fuses with lysosomes, organelles containing digestive enzymes, forming a phagolysosome. Enzymes within the phagolysosome degrade the pathogen.
- Exocytosis: The remnants of the digested pathogen are expelled from the phagocyte.
Why is this Process Considered Nonspecific?
The nonspecificity of phagocytosis stems from the broad recognition of PAMPs. A single PRR can recognize PAMPs from a wide range of pathogens. For example, TLR4 recognizes LPS from various Gram-negative bacteria, while TLR3 recognizes dsRNA from many viruses. This lack of antigen-specific recognition allows phagocytes to respond rapidly to diverse threats without the need for prior exposure to the specific pathogen. This is in stark contrast to the adaptive immune response, which requires clonal selection of specific lymphocytes and takes days or even weeks to develop.
The Role of Inflammation: A Nonspecific Response to Injury
Phagocytosis is often intertwined with inflammation, another crucial nonspecific response. Inflammation is a complex process characterized by redness, swelling, heat, and pain. It's triggered by tissue damage, whether caused by infection or injury. The inflammatory response serves multiple purposes:
- Recruitment of phagocytes: Inflammatory mediators, such as chemokines and cytokines, attract phagocytes to the site of infection or injury.
- Containment of pathogens: Inflammation helps to contain the spread of pathogens by increasing vascular permeability, allowing fluid and immune cells to enter the affected tissue.
- Tissue repair: Inflammation promotes the healing process by stimulating tissue repair and regeneration.
The inflammatory response, while designed to protect the body, can also cause collateral damage. Excessive or prolonged inflammation can contribute to chronic diseases.
Comparing Nonspecific and Specific Immunity
To fully appreciate the nonspecificity of phagocytosis, it's important to compare it to the specific immune response, mediated by lymphocytes (B cells and T cells).
| Feature | Nonspecific Immunity (Phagocytosis) | Specific Immunity (Lymphocytes) |
|---|---|---|
| Response Time | Rapid (minutes to hours) | Slow (days to weeks) |
| Specificity | Broad; recognizes PAMPs | Highly specific; recognizes antigens |
| Memory | No immunological memory | Possesses immunological memory |
| Mechanism | Phagocytosis, inflammation | Antibody production, cell-mediated cytotoxicity |
| Cells Involved | Macrophages, neutrophils, dendritic cells | B cells, T cells |
The specific immune response, while slower to develop, offers long-lasting protection through immunological memory. Upon re-exposure to the same pathogen, the body mounts a faster and more effective response. This is why vaccines work; they introduce weakened or inactivated pathogens to stimulate the adaptive immune response and generate immunological memory.
The Synergistic Relationship: Innate and Adaptive Immunity Working Together
While phagocytosis is a nonspecific response, it plays a critical role in initiating and shaping the adaptive immune response. Phagocytes, particularly dendritic cells, act as antigen-presenting cells (APCs). They process and present antigens to T cells, triggering the activation of specific lymphocytes. This interaction highlights the intricate interplay between innate and adaptive immunity, where the nonspecific response sets the stage for a more targeted and effective specific response. The swift action of phagocytes clears the immediate threat and prepares the ground for the more specialized defenses of the adaptive immune system.
Conclusion: The Essential Role of Nonspecific Phagocytosis
The action of phagocytes, a cornerstone of the innate immune system, is inherently nonspecific. This nonspecificity is not a limitation but rather a crucial feature allowing for rapid and broad-spectrum defense against a vast array of pathogens. The ability to recognize general danger signals (PAMPs) through PRRs ensures prompt action, initiating inflammation and clearing initial infections. While lacking the precision and memory of the adaptive immune response, phagocytosis plays a pivotal role in initiating and shaping the specific immune response, demonstrating the powerful synergy between the innate and adaptive arms of the immune system. Understanding the mechanisms and limitations of phagocytosis provides crucial insight into the overall functioning of our immune system and highlights its incredible complexity and efficiency in protecting us from a constant barrage of microbial threats.
Latest Posts
Latest Posts
-
What Is 1 5 8 As A Decimal
Mar 17, 2025
-
3 Feet 6 Inches In Cm
Mar 17, 2025
-
What Is 26 Out Of 30 As A Percentage
Mar 17, 2025
-
How Many Feet Is 26 In
Mar 17, 2025
-
What Is 6 Out Of 20 As A Percentage
Mar 17, 2025
Related Post
Thank you for visiting our website which covers about Why Is The Action Of Phagocytes Considered A Nonspecific Response . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
