The Entire Responsibility For Urine Formation Lies With The Nephron.
Kalali
Mar 23, 2025 · 7 min read
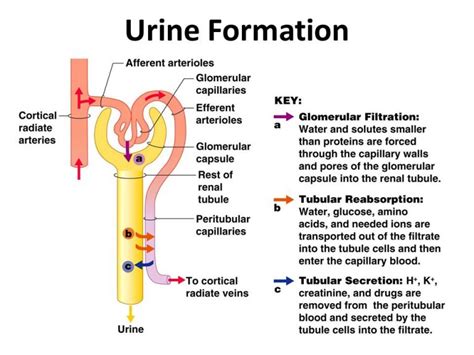
Table of Contents
The Entire Responsibility for Urine Formation Lies with the Nephron: A Deep Dive into Renal Physiology
The human urinary system is a marvel of biological engineering, responsible for maintaining the delicate balance of fluids and electrolytes within the body. At the heart of this system lies the nephron, the functional unit of the kidney. While the kidneys themselves perform the overall task of urine production, the entire responsibility for urine formation rests squarely on the shoulders of the individual nephrons. This article will delve into the intricate processes occurring within the nephron, exploring how it filters blood, reabsorbs vital substances, and secretes waste products to ultimately produce urine.
The Nephron: Structure and Function
Before we explore the processes of urine formation, understanding the nephron's structure is crucial. Each kidney contains approximately one million nephrons, each composed of two main parts: the renal corpuscle and the renal tubule.
The Renal Corpuscle: The Filtration Unit
The renal corpuscle, located in the cortex of the kidney, is responsible for the initial filtration of blood. It consists of:
-
Glomerulus: A network of capillaries where blood is filtered. The glomerular capillaries are fenestrated, meaning they have pores that allow water and small solutes to pass through while retaining larger molecules like proteins and blood cells. The high hydrostatic pressure within the glomerulus is crucial for driving filtration.
-
Bowman's Capsule: A double-walled cup surrounding the glomerulus. The filtrate, the fluid that passes through the glomerular capillaries, enters Bowman's capsule and begins its journey through the renal tubule.
The Renal Tubule: Reabsorption and Secretion
The renal tubule is a long, convoluted tube extending from Bowman's capsule. It is divided into several segments, each with specialized functions in modifying the filtrate:
-
Proximal Convoluted Tubule (PCT): The PCT is the longest and most active segment of the renal tubule. Here, the majority of reabsorption occurs. Essential nutrients like glucose, amino acids, and ions (sodium, potassium, chloride, bicarbonate) are actively transported back into the bloodstream. Water follows passively via osmosis. The PCT also secretes certain substances like hydrogen ions and drugs into the filtrate.
-
Loop of Henle: This loop extends into the medulla of the kidney and plays a crucial role in concentrating urine. The descending limb is permeable to water but less permeable to ions, while the ascending limb is impermeable to water but actively transports ions out of the filtrate, creating a concentration gradient. This countercurrent mechanism is vital for maintaining the osmotic gradient in the medulla, essential for water reabsorption.
-
Distal Convoluted Tubule (DCT): The DCT continues the process of fine-tuning the filtrate's composition. It actively reabsorbs sodium and calcium ions, while secreting potassium and hydrogen ions. The DCT is also influenced by hormones such as aldosterone (regulates sodium reabsorption) and parathyroid hormone (regulates calcium reabsorption).
-
Collecting Duct: Multiple DCTs drain into a collecting duct. The collecting ducts run through the medulla and are influenced by antidiuretic hormone (ADH), also known as vasopressin. ADH increases the permeability of the collecting duct to water, allowing for increased water reabsorption and the production of concentrated urine.
The Three Processes of Urine Formation: A Nephron-Centric View
Urine formation involves three primary processes, all orchestrated by the nephron:
1. Glomerular Filtration: The Initial Sieving
Glomerular filtration is the first step in urine formation. The high hydrostatic pressure within the glomerulus forces fluid and small solutes from the glomerular capillaries into Bowman's capsule. This filtrate contains water, glucose, amino acids, ions, urea, and other small molecules. However, larger molecules like proteins and blood cells are generally prevented from passing through the glomerular filtration membrane due to their size and charge. The glomerular filtration rate (GFR) is a critical measure of kidney function.
2. Tubular Reabsorption: Reclaiming the Essentials
Tubular reabsorption is the selective retrieval of valuable substances from the filtrate back into the bloodstream. This process occurs primarily in the PCT, but also in other segments of the renal tubule. The specific mechanisms of reabsorption vary depending on the substance:
-
Glucose Reabsorption: Glucose is almost entirely reabsorbed in the PCT through a sodium-glucose cotransporter. If blood glucose levels are excessively high (as in diabetes), the transport maximum can be exceeded, leading to glucose appearing in the urine (glycosuria).
-
Amino Acid Reabsorption: Similar to glucose, amino acids are actively reabsorbed in the PCT.
-
Sodium Reabsorption: Sodium reabsorption is crucial for maintaining fluid balance and electrolyte homeostasis. It occurs along the entire length of the renal tubule, regulated by hormones like aldosterone.
-
Water Reabsorption: Water reabsorption follows the movement of solutes, primarily sodium, due to osmotic forces. The majority of water reabsorption occurs in the PCT and the Loop of Henle, influenced by ADH in the collecting duct.
-
Other Substances: Other substances like potassium, chloride, bicarbonate, and phosphate are also reabsorbed in varying degrees throughout the renal tubule.
3. Tubular Secretion: Fine-Tuning the Excretion
Tubular secretion is the process by which substances are actively transported from the peritubular capillaries (the capillaries surrounding the renal tubules) into the filtrate. This process serves several important functions:
-
Eliminating Waste Products: Certain waste products like creatinine and certain drugs are secreted into the filtrate to enhance their excretion.
-
Regulating pH: Hydrogen ions and bicarbonate ions are secreted to regulate blood pH. The kidneys play a crucial role in maintaining acid-base balance.
-
Eliminating Excess Ions: Excess potassium ions and other electrolytes can be secreted to maintain electrolyte balance.
These three processes – glomerular filtration, tubular reabsorption, and tubular secretion – work in concert within the nephron to precisely regulate the composition of the filtrate, ultimately forming urine.
Hormonal Regulation of Urine Formation: A Symphony of Control
Several hormones play crucial roles in regulating urine formation, primarily by influencing sodium and water reabsorption in the nephron:
-
Antidiuretic Hormone (ADH): Released by the posterior pituitary gland in response to dehydration or increased plasma osmolarity, ADH increases water permeability in the collecting duct, leading to increased water reabsorption and the production of concentrated urine.
-
Aldosterone: Released by the adrenal cortex in response to low blood sodium levels or high potassium levels, aldosterone stimulates sodium reabsorption and potassium secretion in the DCT and collecting duct. This helps maintain sodium balance and blood pressure.
-
Atrial Natriuretic Peptide (ANP): Released by the heart in response to increased blood volume, ANP inhibits sodium reabsorption in the collecting duct, promoting sodium excretion and lowering blood pressure.
-
Parathyroid Hormone (PTH): Released by the parathyroid glands in response to low blood calcium levels, PTH increases calcium reabsorption in the DCT.
The interplay of these hormones ensures that urine formation is tightly regulated to maintain the body's fluid and electrolyte balance.
Clinical Significance: Diseases of the Nephron
Dysfunction of the nephron can lead to various kidney diseases, impacting urine formation and overall health. Some examples include:
-
Glomerulonephritis: Inflammation of the glomeruli, potentially leading to decreased GFR and proteinuria (protein in the urine).
-
Acute Kidney Injury (AKI): Sudden loss of kidney function, often caused by ischemia, toxins, or infection.
-
Chronic Kidney Disease (CKD): Gradual loss of kidney function over time, often resulting from diabetes, hypertension, or glomerulonephritis.
-
Polycystic Kidney Disease (PKD): A genetic disorder characterized by the development of cysts in the kidneys, impairing nephron function.
Understanding the intricacies of nephron function is vital for diagnosing and managing kidney diseases.
Conclusion: The Nephron – Master of Renal Physiology
The nephron stands as the fundamental unit responsible for the remarkable process of urine formation. Through the precise coordination of glomerular filtration, tubular reabsorption, and tubular secretion, the nephron maintains the body's fluid and electrolyte balance, eliminates waste products, and contributes to overall health. The intricate mechanisms within the nephron, regulated by hormonal feedback loops, highlight the complexity and efficiency of renal physiology. Further research into nephron function continues to unravel new insights into kidney diseases and develop novel therapeutic strategies. Appreciating the complete responsibility of the nephron for urine formation provides a crucial foundation for understanding the importance of kidney health.
Latest Posts
Latest Posts
-
5 Cups Is How Many Fluid Ounces
Mar 24, 2025
-
Which Of The Following Is A Renewable Resource
Mar 24, 2025
-
How Many Cups Are In 15 Oz
Mar 24, 2025
-
The Normal Pacemaker Of The Heart Is The
Mar 24, 2025
-
400 F Is What In C
Mar 24, 2025
Related Post
Thank you for visiting our website which covers about The Entire Responsibility For Urine Formation Lies With The Nephron. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
